A guide to Pulse Oximetry for first aiders
Many advanced first aiders will be trained to use additional monitoring equipment. In this blog post we discuss the use of pulse oximetry and its common indications and draw backs. 
What is Pulse Oximetry?
Pulse oximetry is a simple non-invasive method of measuring the level of oxygen saturation in arterial blood. It works by assessing the absorption of infra-red light within oxygenated and non-oxygenated haemoglobin within the small arteries, usually in the finger-tip. The pulse oximeter then calculates the percentage of haemoglobin that is oxygenated and displays this as the oxygen saturation level on the screen.
The display will often show the patient’s pulse rate as well.
Normal Pulse Oximetry Readings
In a normally healthy person, the oxygen saturation within their bloodstream spans a very narrow normal range between 94% – 100%. However illness or serious injury can cause these levels to drop quickly:
- 90 – 93% represents evidence of hypoxia
- 85 – 89% represents serious hypoxia
- 85% or less represents critical hypoxia
Hypoxia just means “low oxygen”.
When to use Pulse Oximetry
Pulse oximetry can be used on any patient as part of your patient assessment. Many organisations train pulse oximetry alongside the use of Oxygen therapy (which is outside the scope of this article).
It is especially important to remember to use pulse oximetry and record readings in the following patients:
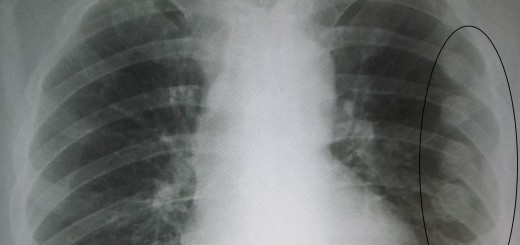
- Respiratory conditions – Asthma / Chronic Obstructive Pulmonary Disease etc.
- Cardiac / heart conditions
- Reduced levels of consciousness
Problems with pulse oximetry
There are several situations where pulse oximetry may not be accurate:
- Irregular heart rhythms
- Thick or dark nail varnish
- Shivering / movement
- Bright light
- Carbon monoxide poisoning
In this situations remember to use your clinical judgement along with the pulse oximetry reading!




Clear and concise