First aid guide to Pulmonary Embolism (PE)
In this blog post we discuss the first aid for Pulmonary Embolism – a blood clot in the lungs!
What is a Pulmonary Embolism (PE)?
Every day the pulmonary capillary bed filters tiny blood clots from the circulation. However, occasionally larger blood clots or other emboli cause obstruction of the pulmonary vessels.
When a blood clot blocks a blood vessel in the lung this is known as a Pulmonary Embolism.
The consequences depend on the size of the emboli and the location where they cause a blockage, and can range from slight breathlessness to sudden cardiac arrest.
What are the signs and symptoms of a Pulmonary Embolism?
The signs and symptoms will usually depend on the emboli size and location of the obstruction:
- multiple small emboli will usually result in progressive shortness of breath over a long period of time;
- larger clot which obstructors a segment of a pulmonary artery may present with pleuritic pain (pain on breathing) and/ or haemoptysis (coughing up blood) with little or no compromise to the circulation;
- a major pulmonary emboli (PE) – a clot which obstructs the larger branches of the pulmonary tree may present with sudden difficulty in breathing, often with a rise in the pulse rate and/ or a fall in blood pressure; and
- massive pulmonary emboli, often presenting with a sudden loss of consciousness, tachypnoea (rapid breathing) and noticeable neck vein distension. These emboli often prove immediately or rapidly (often within the hour) fatal.
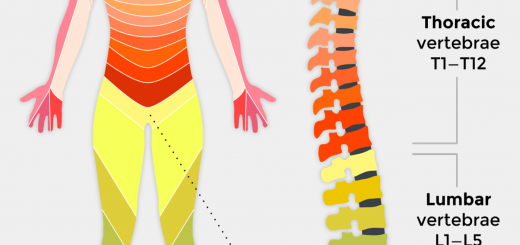
The majority of pulmonary emboli result from thrombi (clots) that originate in the deep veins of the upper and lower limbs and the pelvis.
When a thrombus detaches from its original site, it moves through the venous system to the pulmonary circulation and most often obstructs a major branch of the pulmonary artery.
Symptoms of a PE are (in order of most common):
- dyspnoea (difficulty in breathing);
- tachypnoea (rapid breathing);
- chest pain;
- tachycardia (rapid heart rate);
- cough;
- haemoptysis (coughed up blood or blood streaked sputum); and
- leg pain and/ or deep vein thrombosis (DVT).
The patient may also be exhibiting or complaining of:
- splinting of ribs with breathing (for example, bending over or holding the chest)
- light-headedness or dizziness
- fainting
- sweating
In the majority of instances it occurs as a sudden onset of shortness of breath, either at rest or on exertion. It can present with a range of symptoms but in most instances, patients exhibit one or more risk factors.
What are the risk factors for a Pulmonary Embolism?
Predisposing factors (at least one usually present in 80-90 per cent of all instances of PE) include:
- recent surgery (especially abdominal, pelvic, hip or knee) or post-operative intensive care;
- pregnancy. PE is the leading cause of pregnancy related maternal death in the developed world;
- recent MI (myocardial infarction – a heart attack);
- limb problems, such as recent lower limb fractures, varicose veins or lower limb problems resulting from stroke or spinal cord injury;
- malignancy (cancer), specifically abdominal or pelvic, advanced metastatic disease or concurrent chemotherapy;
- age greater than 40 years, previous PE or DVT, immobility, thrombolic disorders and other recent trauma.
Other risk factors include prolonged air, coach or other travel resulting in prolonged periods of immobility (especially while sitting) and oral oestrogen (for example, contraceptive pills).
What is the first aid for a Pulmonary Embolism?
As with all patients, stepwise assessment and management of the patient’s airway, breathing, circulation and disability should be performed, however, specifically consider:
Breathing. Assess the respiratory rate and effort. Sudden onset breathlessness may be the only symptom of a PE and patients with pre-existing heart failure or pulmonary disease may only notice a worsening of their breathlessness.
Signs and symptoms combined with pre- disposing factors. Patients exhibiting signs or symptoms with predisposing factors should always be suspected of having a PE until proven otherwise.
Lower limbs. Deep Vein Thrombosis (DVT)s can result in unequal or swollen legs that are (sometimes) red and hot to touch. Tenderness and pain may also be present.
First aid treatment is very limited, patients should be rapidly removed to hospital – a high index of suspicion and rapid transport are the key to saving patients with a PE.
FAQs
Can a person survive a pulmonary embolism?
Although pulmonary embolism can be life-threatening, most people do survive it.
Can pulmonary embolism be cured?
Yes, pulmonary embolism can be cured early if it’s treated on time.
Who is at high risk for pulmonary embolism?
Certain medical conditions increase the risk of pulmonary embolism, such as cancer, heart disease, and disorders that affect clotting. Other risk factors include being inactive for long periods, having a blood clot in the leg, smoking, and having a history of stroke or heart failure.
What are the warning signs of a pulmonary embolism?
Some of the warning signs of a pulmonary embolism are chest pain, shortness of breath, and lightheadedness.
How do you prevent pulmonary embolism?
A couple of ways to prevent pulmonary embolism are exercising regularly, maintaining a healthy weight, staying hydrated, and not sitting still for a long time.
Conclusion
If someone suffers from pulmonary embolism, they should ensure to book follow-up appointments with their healthcare provider. Make sure to reach out to your doctor if you experience certain symptoms while taking a blood thinner, such as a bruise that keeps getting bigger or a bad headache.
Being diagnosed early on and getting quick treatment can help those suffering from pulmonary embolism. Stay aware of the symptoms so you can contact your healthcare provider immediately if you’re at a risk of developing pulmonary embolism.





Relieve pressure on the brain.