First Aid For Internal Bleeding
Blood is an incredibly important component of our body. To keep the body functioning and the organs supplied with oxygen, it needs enough circulating blood volume.
Blood consists of red blood cells (erythrocytes), which convey oxygen throughout the body, white blood cells (leucocytes), which fight introduced infection, platelets which assist in the clotting process, and plasma, the fluid portion of blood.
Blood is moved around the body under pressure by the heart and blood vessels. But without adequate blood volume and pressure, the human body soon collapses. Bleeding, or hemorrhage, poses a serious threat by causing both the volume and the pressure of the blood to decrease through blood loss.
Without adequate circulating blood, the body cannot receive a constant supply of oxygen and nutrients. As a result, the organs become damaged.
Bleeding is one of the most common causes of death in accidents. There are two types of bleeding: external bleeding, which is obvious and apparent, and internal bleeding, where the bleeding is not apparent at the outset. However, internal bleeding may show itself later in the form of bleeding from the nose, ear, lungs, or stomach.
What is Internal Bleeding?
Internal bleeding, also known as an internal hemorrhage, is bleeding that occurs in an internal organ. It can happen in almost any organ in the body.
Internal bleeding is due to damage to the blood vessels, usually through some kind of trauma. Our internal organs are packed with tiny blood vessels which receive oxygen and other essential nutrients to keep them functioning as they should. But when internal bleeding occurs, this process is disrupted.
Some types of internal bleeding are considered relatively minor and may resolve themselves. However, others are potentially life-threatening and require urgent medical attention.
What Causes Internal Bleeding?
There are multiple possible causes of internal bleeding, some common and some less common.
Trauma, such as a motor accident or head injury, is one of the most common causes. When blunt force trauma occurs, it puts undue pressure on blood vessels inside the organs.
If the pressure is severe enough, it can cause the vessels to become damaged and bleed out. But internal bleeding isn’t always caused by trauma. Here are some other reasons internal bleeding may occur:
- Peptic ulcers
- GI (gastrointestinal) tumors
- Endometriosis in women
- Ruptured cysts
- Post-surgical bleeding
- Bleeding on the brain, for example, a hemorrhage stroke
- Fractured bones
- A ruptured ectopic pregnancy
- Aortic aneurysms
Factors that increase a person’s risk of internal bleeding include:
- Blood thinning medications
Some prescription medications are designed to thin the blood. These include the common pain relief drug aspirin, the antiplatelet medicine clopidogrel (Plavix), and the anticoagulant coumadin (Warfarin).
- Bleeding disorders
Bleeding disorders such as hemophilia affect the normal clotting process of the blood. This process is known as coagulation. After an injury, a healthy person’s blood quickly begins to clot to prevent blood loss and heal the wound. However, in a person with a bleeding disorder, this process is inhibited, which can lead to excessive bleeding both inside and outside of the body.
- Excessive alcohol consumption
Alcohol thins the blood and prevents it from clotting. This puts heavy drinkers and binge drinkers at an increased risk of internal bleeding.
- NSAIDs
Overuse of NSAIDs (nonsteroidal anti-inflammatory drugs), such as ibuprofen, irritates the gastrointestinal wall. This can lead to the formation of ulcers. If left untreated, these ulcers can cause potentially life-threatening internal bleeding.
- Cancer chemotherapy drugs
Certain chemotherapy agents can suppress bone marrow function, which reduces coagulation and increases the risk of internal bleeding.
Visible and Concealed Internal Bleeding
Internal bleeding is classified as either visible or concealed. Visible internal bleeding can be seen. However, when internal bleeding is concealed, no direct evidence of bleeding is obvious.
Internal bleeding should always be considered serious, and medical attention should be sought immediately.
Does a patient have internal bleeding?
In most instances, obtaining an adequate history of the incident or illness will give the first aider the necessary clues as to whether internal bleeding may be present.
However, remember that current signs and symptoms, or the lack of them, do not necessarily indicate the casualty’s condition.
Certain critical signs and symptoms may not appear until well after the incident due to the stealth of the bleed. Sometimes, they may only be detected by the fact that the casualty’s observations worsen despite there being no obvious cause.
Visible internal bleeding
Visible internal bleeding can vary in appearance depending on the site of the bleeding. Look out for the following:
- Lungs – frothy, bright red blood coughed up by the casualty
- Stomach – a dark matter which looks like coffee grounds coughed up by the casualty or red blood in the vomit
- Intestine/Bowel – dark, loose, foul-smelling stools
- Urinary Tract – dark or red-colored urine
- Ears – bright, sticky blood or blood mixed with clear fluid
- Bruising – the tissues look dark due to the blood under the skin. This is usually caused by blows from blunt instruments or by crushing.
Concealed internal bleeding
In the case of concealed internal bleeding, the first aider is heavily reliant on a patient’s history, signs, and symptoms. Judgment and experience play a part, but it may come down to your ‘gut feeling.’
If you’re unsure, assume the worst and treat for internal bleeding. The detection of internal bleeding relies upon good observations and an appreciation of the physical forces that have affected the casualty.
The symptoms of internal bleeding can look similar to those of a patient suffering from shock.
Here are some signs to look out for:
- Skin appearance: Does the patient have cool, clammy, or unusually pale skin?
- Level of consciousness: Check a patient’s eyes, voice, and motor skills to assess their level of consciousness. See our guide on AVPU and GCS.
- Pulse rate: Check for a weak or rapid pulse. Anything over 100 beats per minute indicates concern.
- Respiratory rate: Check for rapid or shallow breathing.
Other signs and symptoms include:
- Dizziness upon standing
- Low blood pressure
- Severe weakness or fatigue
- Feeling cold, even in a warm environment
- Anxiety and confusion
- Excessive thirst
- Guarding of the abdomen
- Nausea and vomiting
- Visible swelling in the abdomen
- Pain
Internal bleeding of all types is usually accompanied by pain. The main exception to this rule is gastrointestinal bleeding, which is often slower and much more subtle. Diagnostic testing by a medical professional is needed to rule this out. See the section below on GI internal bleeding for more information.
The symptoms above may be present with all types of internal bleeding. However, certain locations of the body present with specific symptoms.
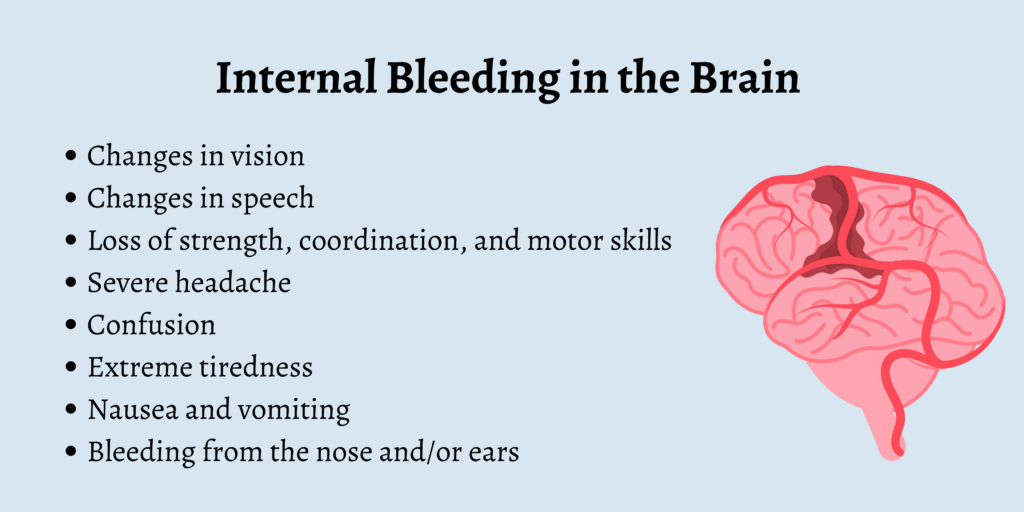
Internal bleeding in the brain
Check for the following symptoms:
- Changes in vision
- Changes in speech
- Loss of strength, coordination, and motor skills
- Severe headache
- Confusion
- Extreme tiredness
- Nausea and vomiting
- Bleeding from the nose and/or ears
Internal bleeding in the chest
Check for the following symptoms:
- Chest pain
- Trouble breathing or shortness of breath
- Rapid shallow breathing
- Rapid heart rate
- Coughing up blood
Internal bleeding in the abdomen
This excludes the signs of gastrointestinal (GI) bleeding (find more information on this below.) For all other bleeding on the abdomen, look out for:
- Pain anywhere in the abdomen region, including the stomach, flank, and pelvis.
- Blood in the urine
- Extreme episodes of vomiting
- Bruising around the abdomen, particularly down the sides and the navel area.
Gastrointestinal bleeding
Gastrointestinal bleeding (GI) bleeding differs somewhat from other types of internal bleeding.
GI bleeding is not normally associated with trauma. Instead, common causes include:
- GI Infections, such as gastroenteritis and colitis.
- Stomach ulcers and other irritations to the lining of the stomach.
- Inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease.
- Diverticular disease: a relatively common condition where small pouches push out through the walls of the intestines.
- Excessive alcohol consumption that can lead to ruptured blood vessels in the stomach and the esophagus.
- Hemorrhoids that become irritated or inflamed.
- Anal fissures and anal abscesses.
- A rare condition called ischemic colitis.
- Bowel, colon, or rectal cancer.
Signs and symptoms of GI bleeding
As we mentioned earlier, unlike other forms of internal bleeding, bleeding which originates in the gastrointestinal tract is often painless. So, it’s important to know the other signs and symptoms to look out for. These include:
- Visible blood in the stool. This can appear as bright red, rusty brown, or dark, black, and tarry.
- Visible blood in the toilet bowl after emptying the bowels.
- Nausea and vomiting.
- Blood in the vomit.
- Loss of appetite.
First aid for Internal Bleeding
If internal bleeding from any cause is suspected, it’s important to act quickly.
Here are the steps you should take if you suspect a patient is suffering from internal bleeding.
- Call for emergency medical help
- Perform a primary survey
- If conscious, treat the patient for shock
- If unconscious, put them into the recovery position
- Treat any injuries found
- Provide reassurance while you wait for emergency medical help
Conclusion
Internal bleeding has a wide variety of causes, and the severity of the condition can vary from mild to life-threatening.
As a first aider, knowing the signs and symptoms to look out for is crucial when it comes to delivering care for a patient. So, be sure to familiarize yourself with the information above so that you can be ready to act in an emergency.