How to assess cardiac chest pain

When assessing chest pain it is important to find out the following information
Time of onset
When was the pain first noticed? What was the patient doing at the time? Has there been any trauma to have caused the pain and is there pain on pressing the chest wall (unlikely to be cardiac in origin)?
Time of worst pain
When was the pain at its worst? Has the pain changed in nature or severity? Was the onset sudden (usually non-cardiac), or did it gradually build up, if so over how a long period of time? If the pain has eased, did anything cause the reduction, for example position or medications?
Breathlessness
Is the patient short of breath? Can the breathlessness by relieved by a change in position? Is the patient pale or cyanosed?
Has there been any recent history of breathlessness (esp. on exertion)? Are there any other known causes for the breathlessness such as Chronic Obstructed Pulmonary Disease (COPD) or a recent chest infection?
Does the pain change in nature or severity with deep breaths (unlikely to be cardiac)? Is there a cough? If so, is it productive? (yellow, brown or green sputum can indicate a chest infection, while white frothy sputum − possibly blood tinged − is indicative of fluid backup in the lungs from heart failure).
Nausea and vomiting
Does the patient feel sick, if so for how long and have they vomited? (Nausea is one of the symptoms of a myocardial infarction, but it can be a symptom of gastric reflux or indigestion).
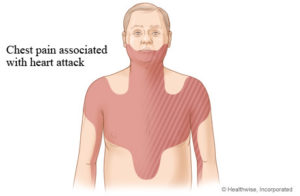
Character of pain and radiation
Is the pain central, sub-sternal or described as a heavy weight or tightness across the chest? (Pain that can be localised to beneath one or two fingers is unlikely to be cardiac in origin and cardiac pain is usually central and sub-sternal rather than lateral)
Does the pain radiate into the arms, back, neck or jaw? Get the patient to score the pain out of ten, with ten being the worst. This can help to monitor changes in pain severity.
Cardiac risk factors
Does the patient have any cardiac risk factors, for example, smoking, diabetes, hypertension, family history of heart disease, obesity, heavy alcohol consumption, lack of exercise and the contraceptive pill, etc. While having any of these factors does not mean that the chest pain is cardiac in origin, it can make it more likely.
Has this patient had this type of pain before? Is there a history of heart disease, previous infarctions or surgery such as a bypass?
Medications
What medications is the patient taking? Have they been compliant with their doses? Has any medication been changed recently? Do they have any problems when they do or do not take their medication? Drugs such as beta blockers, digoxin or aspirin can indicate a pre-disposition to heart disease of some sort.
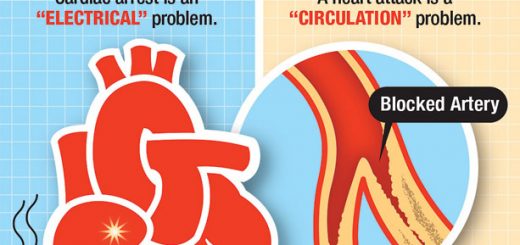
Recognising a heart attack
Signs and symptoms of a heart attack (myocardial infarction) commonly include central, sub-sternal chest pain which may radiate into the left or right arm, neck, back and jaw. Pain is usually unaltered by movement, respiration or the position of the patient. The patient can also complain of difficulty in breathing, nausea, hypotension, diaphoresis (sweating) and restlessness.
These signs and symptoms are only typically representative of cardiac related chest pain, each patient can exhibit different signs and symptoms. Careful history taking and patient examination are essential in determining the possible causes of chest pain.